What is a retinal detachment?
The retina lines the inside of the eye like wallpaper. A retinal detachment develops when the retina pulls away from its normal position.
What are the symptoms of retinal detachment?
Symptoms of retinal detachment include painless floaters, flashing lights, and a curtain of visual loss that spreads across the field of vision. Vision loss can progress rapidly. Untreated, retinal detachment usually causes permanent blindness.
What causes a retinal detachment?
 Breaks in the retinal tissue (retinal holes and retinal tears) are normally found in approximately 10% of people. In a small minority of persons with retinal breaks, liquid vitreous leaks beneath the retina, separating it from the eyewall and causing a retinal detachment. A sudden separation of the vitreous from the retina (posterior vitreous detachment) is often the inciting event causing a retinal break or detachment. Macular pucker can also develop following a vitreous detachment.
Breaks in the retinal tissue (retinal holes and retinal tears) are normally found in approximately 10% of people. In a small minority of persons with retinal breaks, liquid vitreous leaks beneath the retina, separating it from the eyewall and causing a retinal detachment. A sudden separation of the vitreous from the retina (posterior vitreous detachment) is often the inciting event causing a retinal break or detachment. Macular pucker can also develop following a vitreous detachment.
Who gets retinal detachment?
Retinal detachment develops in approximately 1 in 10,000 people per year. Certain conditions increase the likelihood of retinal detachment, including acute symptomatic retinal breaks, acute posterior vitreous detachment, nearsightedness, eye injury, eye surgery, or a history of retinal detachment in family members. Lattice degeneration, occurring in 10% of people, is found in one-third of eyes with retinal detachment. If a person has a retinal detachment in one eye, there is a 10% chance of eventually developing a detachment in their other eye.
How is a retinal detachment diagnosed?
Anyone who has sudden flashes, floaters, or peripheral vision loss needs an urgent examination by an eye doctor familiar with retinal diseases. A careful dilated retinal examination is necessary to diagnose retinal breaks or detachment.
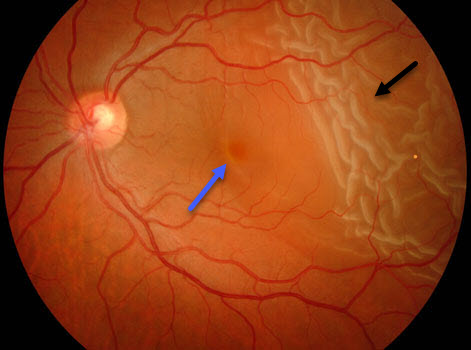
A retinal detachment (black arrow) just extends thru the macula (blue arrow)
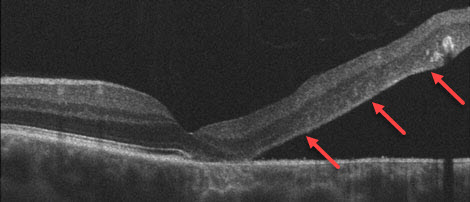
OCT scan shows the retina lifting away from the eyewall
How are retinal breaks and detachment treated?
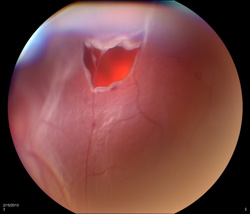
Retinal breaks
Asymptomatic retinal breaks or lattice degeneration in low-risk eyes do not require treatment. Eyes with symptomatic breaks need preventive treatment. High-risk eyes with asymptomatic breaks are often treated as well. “Gluing” the surrounding retina with heat (laser photocoagulation) or cold (cryotherapy) usually prevents retinal detachment from developing.
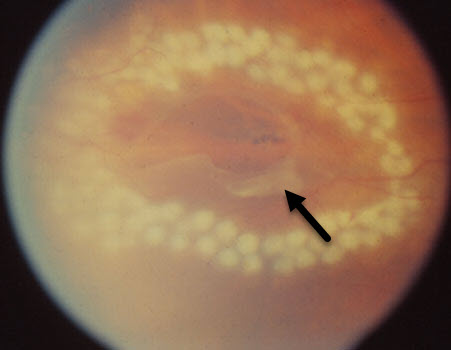
White laser photocoagulation spots surround a retinal tear (arrow)Retinal detachment
Once the retina separates from the eyewall it must be surgically pushed back into place; the causative retinal breaks are then “glued” with laser photocoagulation or cryotherapy. There are several surgical options available for repairing retinal detachment. Scleral buckling pushes the “wall against the wallpaper” whereas pneumatic retinopexy and vitrectomy push the “wallpaper against the wall.” Surgery is usually performed within a day or two of diagnosis, particularly if the macula and central vision are not yet affected.
Scleral buckle
Scleral buckling is an outpatient procedure performed in the operating room under local anesthesia. A piece of silicone rubber is permanently sewn to the outside of the eye, pushing (or “buckling”) the eyewall (sclera) against the retinal breaks. The eye looks and feels normal following surgery. Scleral buckling successfully re-attaches in the retina in 80-90% of eyes with one operation.
Pneumatic Retinopexy
Pneumatic retinopexy is a painless in-office procedure for repairing selected retinal detachments. After a gas bubble is injected into the eye, the patient positions their head so the bubble floats up against the retinal detachment. Once the retina re-attaches, usually within several days, the causative retinal breaks are surrounded with laser photocoagulation or cryotherapy.
Pneumatic retinopexy has a 75% success rate following placement of the initial bubble. Initial failures are primarily due to poor patient compliance with head positioning or the development of new retinal breaks. Subsequent surgery (i.e. scleral buckling or vitrectomy) is usually successful in re-attaching the retina.
Vitrectomy
Vitrectomy is an outpatient surgery performed in the operating room under local anesthesia. The vitreous is removed, directly eliminating the retinal traction on the causative retinal breaks. Scar tissue growing over the retinal surface can be removed as well. The eye is then filled with a gas bubble. This mechanically pushes the retina back against the eyewall. Laser photocoagulation or cryotherapy is then used to seal the retinal breaks. A scleral buckle is sometimes also performed at the time of vitrectomy.
Patients often need to maintain certain positioning (look down, sleep on their side, and/or avoid sleeping on their back), avoid driving to higher altitudes and avoid airplane flying for several months following surgery. These restrictions are due to positioning the gas bubble so it floats up against the retina to help hold it against the eyewall and to prevent the bubble from expanding at higher altitudes. Even if the eye will ultimately see well, vision will be quite poor for a few months since the eye is not designed to see well through the bubble. If the retina remains attached as the bubble absorbs, vision improves within a few months.
Vitrectomy surgery has an 80-90% success rate with one operation. Some eyes require multiple procedures, and rarely some detachments cannot be repaired.
Watch an actual vitrectomy for retinal detachment.
Will my vision improve after retinal reattachment surgery?
The most important factor predicting final eyesight is the vision immediately before surgery. If the vision is initially good, successful surgery generally yields good sight. However, if the central vision is poor pre-operatively, final vision is often decreased even with successful retinal reattachment.
Patients usually need to have their glasses changed several months after retinal reattachment surgery, particularly following scleral buckling. Final vision may also be decreased by the later development of a cataract, which often follows vitrectomy surgery. Cataract surgery is often successful in restoring vision in such cases.
View more retina images at Retina Rocks, the world’s largest online multimedia retina image library and bibliography repository.



