Age-related macular degeneration can be thought of as wearing out of the macula, the small, specialized area of the retina that gives us our straight-ahead reading and driving vision. There are two basic types of macular degeneration. The majority of patients have a less severe dry type, which consists of small aging spots (drusen) in the macula. New blood vessel growth beneath the macula (macular neovascularization) is associated with the wet type. These vessels cause the macula to swell with fluid and blood and often lead to permanent central vision loss.
Since this disease does not affect the part of the eye responsible for side vision, patients never go completely blind. In fact, most people with macular degeneration will see normally throughout their lifetime. However, some may develop blurriness or distortion. In extreme cases, central vision may even be lost.
At this time there is no cure for macular degeneration, although early detection and treatment have been shown to slow or halt the disease. The specialists at Bennett & Bloom Eye Centers are committed to keeping up with the latest technology and treatment options to provide you the best possible outcome. When diagnosed in time, we are often able to treat the condition and help prevent vision loss.
See a television interview from Fox 41 with Dr. Bloom describing macular degeneration.
What is age-related macular degeneration?
Many people, usually after age 65, develop a “wearing out,” or degeneration of the macula as part of the aging process. We don’t know why some people get these changes and others do not. There appears to be an increased risk of age-related macular degeneration (AMD) with increasing age, in cigarette smokers, and in those who have other family members affected by this disease. There are 15 million people in the United States affected by AMD, with over 1.6 million having the more severe wet type.
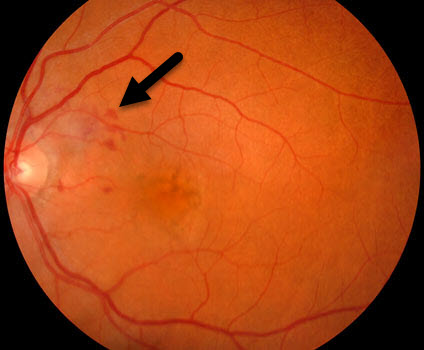
There are two basic types of AMD, dry and wet. The vast majority of people have a less severe dry type. The hallmark clinical finding of dry AMD consists of small aging spots or drusen.
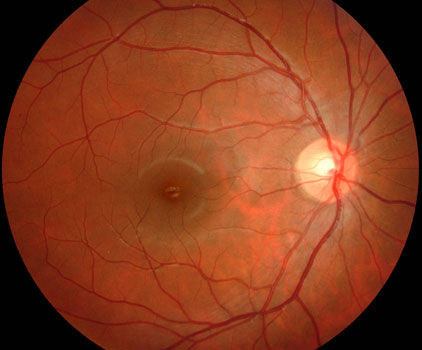
Normal macula
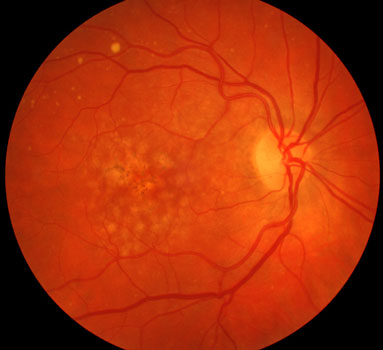
Dry AMD with drusen (yellow spots)
Eyes with geographic atrophy, a variant of dry AMD, develop a wearing away of the macular pigmented tissues. The atrophy causes discrete islands of blind spots. Vision is good unless the atrophy extends into the macular center. Two drugs, Syfovre and Iverzay , were recently approved for geographic atrophy. However, we feel the potential benefits are minimal, and the risks including macular neovascularization and infection, are too signficant to generally recommend these for our patients.
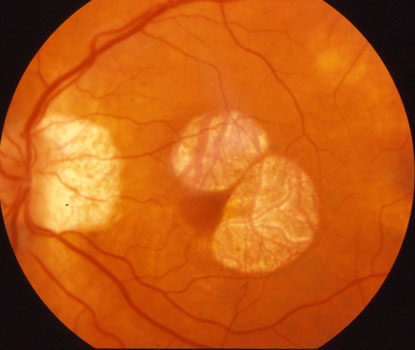
Geographic atrophy just spares the macular center
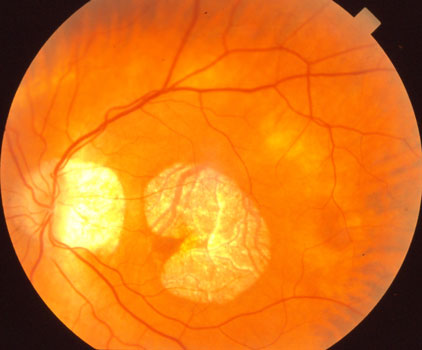
The atrophy gradually enlarged, causing loss of central vision
Some patients with AMD can develop a blister, which is called a retinal pigment epithelial (RPE) detachment. These blisters often cause blurriness or distortion. The blisters can remain stable, spontaneously flatten, or can go on to develop associated macular neovascularization. Treatment with anti-VEGF injections can sometimes make these blisters go away.
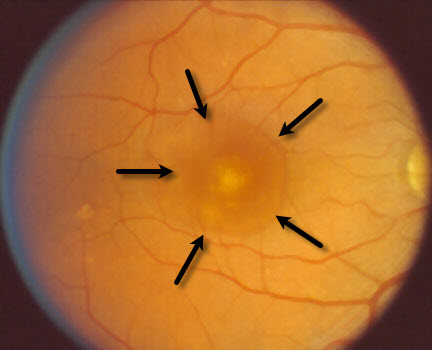
Pigment epithelial detachment (outlined by arrows)
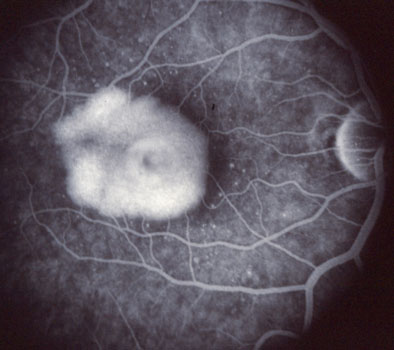
Fluorescein angiogram highlights the blister
New blood vessels (macular neovascularization, MNV) grow beneath the macula in the more severe wet form. These vessels cause the overlying macula to swell with fluid and blood which often causes permanent central vision loss. There are many causes of MNV including angioid streaks, choroidal rupture, degenerative myopia, idiopathic and ocular histoplasmosis.

End-stage wet AMD with macular hemorrhaging and scarring
Macular neovascularization is often invisible without special testing including fluorescein angiography and OCT scanning.
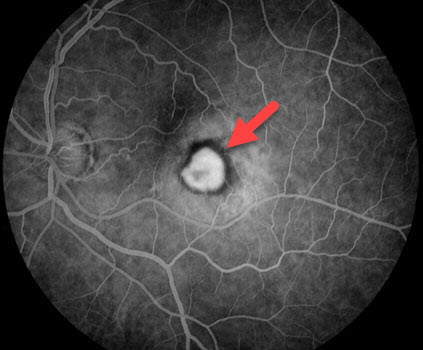
Fluorescein angiography shows a white, well-defined MNV
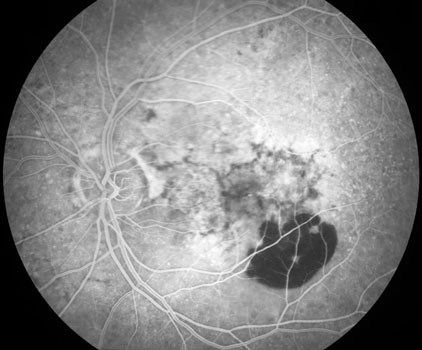
Angiography shows a poorly-defined MNV with no distinct white lesion
What are the symptoms of age-related macular degeneration?
Patients with mild dry AMD usually notice minimal changes in their vision although there may be slow loss of reading vision over many years. If the wet form develops, leakage and bleeding may involve the macular center causing symptoms such as distortion and vision loss. Patients never go completely blind since the part of the eye responsible for peripheral (side) vision is not affected by this disease.

Normal vision

Vision with macular degeneration
 Some patients who lose central vision will see things that aren’t there. These visual hallucinations are known as the Charles Bonnet Syndrome. Although the exact cause is not known, it is thought to represent an attempt of the brain to obtain clear images of things that the macula is no longer supplying. It is not a sign of dementia. This common syndrome was initially described in 1760 by Swiss naturalist Charles Bonnet. His grandfather, blind from cataracts, saw “figures of men, of women, of birds, of carriages, of buildings, etc. He sees these figures make various movements: getting closer, going away, fleeing, diminishing or increasing in size, appearing or disappearing; he sees the buildings rise in front of his eyes…The tapestries in his apartment appear to change suddenly; these tapestries cover themselves with painting displaying different landscapes…All these visions appear to him in perfect clarity and affect him as strongly as if the objects themselves were present…” It requires no treatment other than to reassure the patient that this is not uncommon in those who lose central vision.
Some patients who lose central vision will see things that aren’t there. These visual hallucinations are known as the Charles Bonnet Syndrome. Although the exact cause is not known, it is thought to represent an attempt of the brain to obtain clear images of things that the macula is no longer supplying. It is not a sign of dementia. This common syndrome was initially described in 1760 by Swiss naturalist Charles Bonnet. His grandfather, blind from cataracts, saw “figures of men, of women, of birds, of carriages, of buildings, etc. He sees these figures make various movements: getting closer, going away, fleeing, diminishing or increasing in size, appearing or disappearing; he sees the buildings rise in front of his eyes…The tapestries in his apartment appear to change suddenly; these tapestries cover themselves with painting displaying different landscapes…All these visions appear to him in perfect clarity and affect him as strongly as if the objects themselves were present…” It requires no treatment other than to reassure the patient that this is not uncommon in those who lose central vision.
Patients are often asked to check their central vision every day with an Amsler grid. This grid is a pattern that resembles a checkerboard. You should cover one eye and stare at a black dot in the center of the grid. While staring at the dot, you may notice that the straight lines in the pattern appear wavy to you. You may notice that some of the lines are missing. These may be signs of wet AMD.
Click here to view or download a full-sized Amsler grid for yourself.
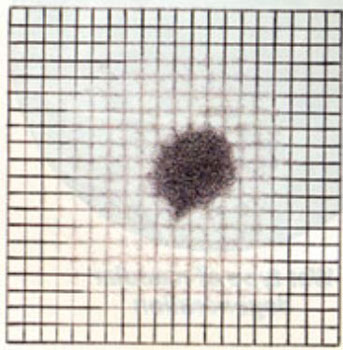
Blurry areas and black spots
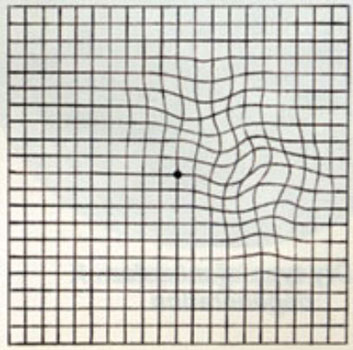
Wavy or crooked lines
How is age-related macular degeneration diagnosed?
The most important step in accurately diagnosing AMD is a careful dilated eye examination by an eye doctor familiar with this disease. Further testing, including OCT scanning and fluorescein angiography, may be necessary.
What treatments are available for age-related macular degeneration?
Preventive treatments.
Nutritional supplements.
The Age-Related Eye Disease Study (AREDS), a large, randomized, multicenter prospective study sponsored by the National Eye Institute, found that taking supplements containing high levels of antioxidants and zinc significantly reduced the risk of advanced AMD. The nutrients are not a cure for AMD, nor will they restore vision already lost from the disease. However, they play a key role in helping people at high risk for developing advanced AMD keep their vision. People who are at high risk for developing AMD should consider taking the formulation used in the study and eating a diet high in vitamin C, vitamin E, zinc, and carotenoids. Your eye doctor will tell you if you would benefit from these supplements based on a dilated eye examination.
AREDS researchers found that people at high risk for developing advanced stages of AMD lowered their risk by about 25 percent when treated with a high-dose combination of vitamin C (500 mg), vitamin E (400 IU), beta-carotene (15 mg), zinc (as 80 mg zinc oxide), and copper (2mg cupric oxide which was also added to prevent a zinc-induced copper deficiency which may be associated with high levels of zinc supplementation). This treatment also reduced the risk of vision loss by about 19 percent. The supplements did not provide any apparent benefit for those with either early AMD (those with either several small drusen or a few medium-sized drusen in one or both eyes) or no AMD.
The AREDS2 evaluated the benefits of adding lutein (10 mg/day) and zeaxanthin (2 mg/day) or omega-3 long-chain polyunsaturated fatty acids (1 gram/day) to the original AREDS formula. None of these lowered the risk of disease progression. However, trial participants who took the AREDS supplement containing lutein/zeaxanthin and no beta-carotene had a slight reduction in the risk of advanced AMD when compared to those who took AREDS with beta-carotene. Also, for a subgroup of participants with very low levels of lutein/zeaxanthin in their diet, adding these supplements to the AREDS formulation helped lower their risk of advanced AMD. There were no significant changes in the effectiveness of the formulation when they removed beta-carotene or lowered zinc. Finally, former smokers who took AREDS with beta-carotene had a higher incidence of lung cancer. The AREDS2 investigators, therefore, suggested replacing the beta carotene in the original formula with lutein and zeaxanthin.
 Supplements based on the AREDS2 study are widely available over the counter and on the internet. Unfortunately, most of these contain a seemingly endless subtle variation in the recommended AREDS ingredients to the point where it is nearly impossible to tell which product has the correct formula. For this reason, we recommend that our patients purchase Bauch + Lomb’s PreserVision AREDS2 Formula which is widely available at any pharmacy for about $25 to $30 for a 2-month supply.
Supplements based on the AREDS2 study are widely available over the counter and on the internet. Unfortunately, most of these contain a seemingly endless subtle variation in the recommended AREDS ingredients to the point where it is nearly impossible to tell which product has the correct formula. For this reason, we recommend that our patients purchase Bauch + Lomb’s PreserVision AREDS2 Formula which is widely available at any pharmacy for about $25 to $30 for a 2-month supply.Some people with intermediate AMD may wish to consider whether or not they wish to take large doses of the supplements for medical reasons. For example, beta-carotene (which is present in the original AREDS formula) has been shown to increase the risk of lung cancer among smokers. Taking supplements with zinc may cause a copper deficiency. The study also found high zinc levels were associated with genitourinary tract problems. Patients may want to discuss the best combination of supplements to take with their primary care physician.
Diet and Lifestyle modifications
Discontinuing smoking, weight loss, eating a heart-healthy diet, and regular exercise appear to be both good for your heart and your eyes. Although not a replacement for AREDS 2 supplementation, here’s a list of various foods rich in vitamins C and E, zinc and carotenoids:
Vitamin C: Oranges, grapefruit, melon, broccoli.
Vitamin E: Whole grains, wheat germ, sunflower oil, safflower oil, canola oil, olive oil, sunflower seeds, almonds, hazelnuts/filberts, peanuts, cashews, walnuts, spinach, avocado, mango, blueberries, beans.
Zinc: Oysters, beef, chicken, pork, lamb, flounder, sole, sardines, cashews, walnuts, pumpkin seeds, sesame seeds, beans, dairy products.
Carotenoids: Fruits (grapes, oranges, apples, apricots, kiwis, mangoes, peaches, nectarines, cantaloupe, honeydew, melon, grapefruit), vegetables (kale, collard greens, spinach, mustard greens, broccoli, green lettuce, peas, Brussels sprouts, squash, yellow pepper, corn, carrots), and other (tomato juice, orange juice).
Laser photocoagulation.
A retinal laser is an instrument that produces a pure, high-intensity beam of light energy. The laser light can be focused onto the retina, selectively treating the desired area while leaving the surrounding tissues untouched. The absorbed energy heats, or photocoagulates, the retina creating a microscopic spot.
Laser surgery is performed in our office while you are awake and comfortable. The laser is used to seal the leaking vessels beneath the retina. The laser treatment usually takes less than 15 minutes to complete, and you can go home immediately following surgery. Arrangements for transportation should be made in advance since you may not be able to drive right away.
Macular neovascularization with surrounding hemorrhage
Dry laser scar following successful laser photocoagulation surgeryLaser surgery was the only treatment for wet AMD from the early 1970s until the early 2000s. Although it decreased the risk of severe central vision loss, most patients couldn’t be effectively treated since it could only be performed for those with well-defined macular neovascularization outside the macular center. Since the vast majority of patients have poorly-defined neovascularization beneath the macular center, most either could not be treated or eventually lost central vision from recurrent central macular bleeding. Since the early to mid-2000s, photodynamic therapy and anti-VEGF agents have virtually replaced laser surgery for treating wet AMD.
Photodynamic therapy.
Laser photocoagulation surgery has traditionally been the standard treatment for patients with wet AMD and macular neovascularization outside the macular center. When macular neovascularization is beneath the center of the macula, laser not only destroys these abnormal vessels but also permanently damages the overlying retina. Patients are thus left with a dry scar but no central vision. Photodynamic therapy, which became available in 2000, was the first treatment that allowed treatment of these central lesions while minimizing retinal damage. The treatment involves injecting Verteporfin (Visudyne) intravenously, followed by a painless treatment utilizing the Zeiss VISULAS 690 laser. Direct daylight exposure within the first 48 hours can cause a severe skin burn, so patients need to remain inside for two days following treatment. Photodynamic therapy is painless and is associated with minimal to no side effects. It usually needs to be repeated every 3 months for multiple treatments for recurrent neovascularization.
Although photodynamic therapy is able to effectively treat most patients with wet AMD, most still lose a moderate amount of vision and vision rarely improves significantly. The emergence of VEGF inhibitors in the mid-2000s has mostly replaced photodynamic therapy as the primary treatment for this disease. It is still used for a small subset of patients who fail to respond to anti-VEGF therapy or as a means to limit the number of anti-VEGF injections.
Vascular Endothelial Growth Factor (VEGF) and Ang-Tie Inhibitors.
In 1989 scientists identified a growth factor (vascular endothelial growth factor, or VEGF) that plays a major role in stimulating new blood vessel growth. Acting like a biologic fertilizer, VEGF causes the cells that line blood vessels (vascular endothelium) throughout the body to multiply and form new vessels. In the macula, VEGF is produced in response to inflammation and lack of oxygen. VEGF binds to the choroidal endothelial cells, which then proliferate to form macular neovascularization. Blocking the VEGF molecule is currently the most effective treatment for macular neovascularization.
In the mid-2000s anti-VEGF drugs became available for treating wet AMD. By binding and blocking the action of VEGF, VEGF-inhibitors act like Roundup, causing neovascularization to involute. Almost overnight they turned a previously and virtually untreatable disease into one that could be successfully controlled with ongoing treatment. Vision is stabilized in well over 90% of eyes and most patients gain several lines of vision. Since their introduction, these drugs have decreased the incidence of AMD-related blindness by nearly 50%.
These medications are injected into the eye in a relatively painless in-office procedure. Lucentis, Eylea and Beovu are the VEGF-inhibitors currently FDA approved for ocular use. Avastin, another VEGF inhibitor initially approved for the treatment of colorectal cancer, is also widely used off-label. Another drug, Vabysmo, inhibits both VEGF and Ang-2, another pathway responsible for new blood vessel growth. All 5 drugs are relatively equally effective in treating wet AMD. The choice of which drug to use is complex and individualized for each patient. Patients initially receive monthly injections until the macular leakage is controlled. The disease process is not cured with these drugs since most patients require maintenance injections every one to three months indefinitely to maintain their vision.
Subretinal surgery.
Using advanced microsurgical techniques, hemorrhage and abnormal blood vessels growing beneath the macula can be removed. These techniques can benefit only a small minority of patients with wet AMD and carry a risk of major complications such as retinal detachment and total blindness. The Submacular Surgery Trial, the definitive National Eye Institute-sponsored study, unfortunately, failed to show any significant benefits for these techniques.
Implantable Miniature Telescope (IMT).
 The Implantable Miniature Telescope (IMT), a pea-sized lens inserted into the eye during a cataract-like operation, was approved for use in patients in 2010. Acting like a telescope, this device enlarges images by about 2 to 3 times, making it easier for those who have already permanently lost central vision to recognize images at distance. One-year efficacy data from a prospective, multicenter trial showed patients had a mean improvement of over 3 lines of vision at both distance and near and three-quarters went from severe to moderate vision impairment. The main complication was clouding of the cornea, with 4% of patients requiring corneal transplant surgery. Persons eligible to receive the telescope need to be over 65 years of age without prior cataract surgery and stable severe to profound vision impairment (best-corrected distance visual acuity 20/160 to 20/800) due to end-stage AMD. Preoperatively patients need to go through the CentraSight Treatment Program to ensure that they are good candidates for this surgery. On July 6, 2017, Bennett & Bloom performed the first IMT surgery in our multi-state region.
The Implantable Miniature Telescope (IMT), a pea-sized lens inserted into the eye during a cataract-like operation, was approved for use in patients in 2010. Acting like a telescope, this device enlarges images by about 2 to 3 times, making it easier for those who have already permanently lost central vision to recognize images at distance. One-year efficacy data from a prospective, multicenter trial showed patients had a mean improvement of over 3 lines of vision at both distance and near and three-quarters went from severe to moderate vision impairment. The main complication was clouding of the cornea, with 4% of patients requiring corneal transplant surgery. Persons eligible to receive the telescope need to be over 65 years of age without prior cataract surgery and stable severe to profound vision impairment (best-corrected distance visual acuity 20/160 to 20/800) due to end-stage AMD. Preoperatively patients need to go through the CentraSight Treatment Program to ensure that they are good candidates for this surgery. On July 6, 2017, Bennett & Bloom performed the first IMT surgery in our multi-state region.
Investigational Treatments.
Although there have been great strides over recent years in treating AMD, we are still far from being able to prevent AMD from developing in the first place, as well as curing macular neovascularization once it develops. There are a multitude of new treatments being investigated, although we will not know if they are helpful or harmful until ongoing clinical studies are completed.
What happens if I lose my reading vision?
Except for airplane pilots, military personnel, etc., most patients who lose reading vision in one eye continue their normal lifestyle without change. Patients should be able to drive a car as long as their vision in the other eye is at least 20/60 in Kentucky and 20/40 in Indiana and Ohio.
Low Vision services and examination.
We may recommend that you see a specialist for a low vision examination. Magnifying lenses or other devices can be prescribed to help with reading and other central vision tasks.For those living in the Kentuckiana and Northern Kentucky areas, the Kentucky Office for the Blind, the Cincinnati Association for the Blind and Visually Impaired, Free Kentucky Talking Book Library Service, and the American Printing House for the Blind offer a myriad of services and resources to help those with vision loss function better and remain independent.
Radio Eye is a non-profit 24-hour radio service that broadcasts the reading of current newspapers and other everyday literature, offering greater independent living to people who are blind, visually impaired or physically handicapped. Radio Eye radio listeners hear the reading of dozens of newspapers, magazines, health materials, grocery ads and much more. The audio stream can be accessed on a special (free) Radio Eye radio, on Library Channel 20 on Lexington Insight Cable TV, in area homes and hospitals, as well as on their website.
Lighthouse Guild is a leading nonprofit vision and healthcare organization, with a long-standing heritage of addressing the needs of people who are blind or visually impaired, including those with multiple disabilities or chronic medical conditions. Through the integration of vision and healthcare services and the expansion of access through education and community outreach, their innovative and comprehensive approach helps people achieve and maintain the highest possible level of function and independence.
What are the chances of my other eye developing wet age-related macular degeneration?
Patients who have no signs of abnormal blood vessels in either eye have a minimal chance of losing central vision. This risk is increased, however, if abnormal blood vessels have already affected one eye. The yearly risk for the second eye becoming involved increases to approximately 1 in 20.
What can I do to prevent vision loss?
There is nothing that any of us can do to prevent our eyes from aging. Vitamin supplements are helpful in decreasing the risks of vision loss and wet AMD from developing in high-risk eyes. The most important thing is to check the central vision of each eye every day and have frequent, regular eye examinations. Any sudden change in the vision requires an immediate examination by your eye doctor.
View more retina images at Retina Rocks, the world’s largest online multimedia retina image library and bibliography repository.



