The retina is nourished by tiny blood vessels that bring blood into (arteries) and out of (veins) the eye. Occasionally an artery will compress the underlying vein, making it difficult for blood to exit the eye. This blockage, called a branch retinal vein occlusion, causes the vein to dilate and leak fluid and blood. The main vein exiting the eye can also become blocked within the optic nerve, causing a central retinal vein occlusion. Retinal vein occlusions are more common in older individuals as well as persons with hypertension, diabetes, or glaucoma.
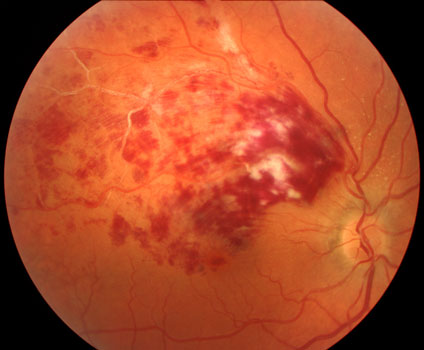
Branch retinal vein occlusion
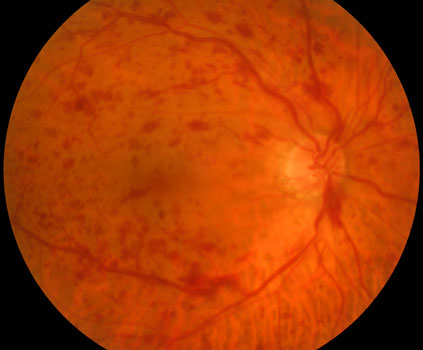
Central retinal vein occlusion
Macular edema develops when the occlusion involves the macula, causing it to swell with fluid and blood. Central vision can become blurred, just as a water droplet placed on a photograph will cause the picture to blister and become distorted. Macular edema develops in 60% of branch retinal vein occlusions and virtually all central retinal vein occlusions.
Retinal vein occlusions can also decrease the overall retinal blood supply. Some eyes will develop tiny new blood vessels along the retinal surface in an attempt to increase the retinal blood supply (retinal neovascularization). These new vessels do not help the eye, however. They are fragile and can cause blindness by bleeding (vitreous hemorrhage) or retinal detachment. Retinal neovascularization develops in about 25% of eyes with branch retinal vein occlusions and rarely in eyes with central retinal vein occlusion.
Eyes with central retinal vein occlusion are classified into the non-ischemic (good retinal arterial circulation) and ischemic (poor circulation) types. Up to two-thirds of eyes with ischemic central retinal vein occlusion (compared with virtually none of the non-ischemic occlusions) develop new blood vessels on the surface of the pupil (iris neovascularization). Iris neovascularization usually develops within the first six months of the occlusion. These vessels can block the outflow of fluid from the eye, causing pain with very high pressures inside the eye (neovascular glaucoma).
What are the symptoms of a retinal vein occlusion?
Retinal vein occlusions can cause painless blurring of the central and peripheral vision. Central retinal vein occlusions generally cause more severe vision loss when compared to branch retinal vein occlusions. Patients may be completely asymptomatic, especially when the other eye sees normally. Neovascular glaucoma can cause severe eye redness, pain, nausea, and total blindness.
How is a retinal vein occlusion diagnosed?
You can’t diagnose a retinal vein occlusion by looking in the mirror since your eye will usually look and feel normal. The diagnosis is made with a thorough retinal examination through a dilated pupil. Additional testing, including OCT scanning and fluorescein angiography, may be performed to better diagnose and assess the need for treatment.
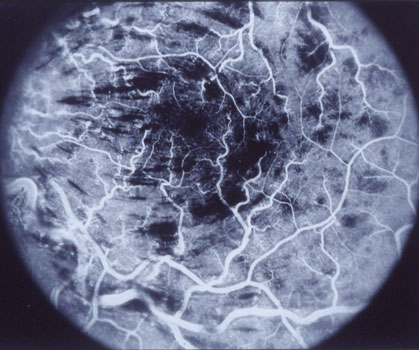
Fluorescein angiogram of a non-ischemic central retinal vein occlusion.
The white dye fills the capillaries between the larger retinal vessels.
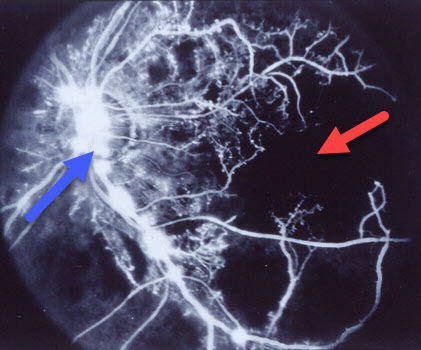
Fluorescein angiogram of an ischemic central retinal vein occlusion shows near total capillary loss (red arrow), along with leakage from retinal neovascularization (blue arrow).
What treatments are available for retinal vein occlusions?
Branch retinal vein occlusion.
Macular edema
- Laser Photocoagulation
A laser is an instrument that produces a pure, high-intensity beam of light energy. The laser light can be focused onto the retina, selectively treating the desired area while leaving the surrounding tissues untouched. The absorbed energy heats, or photocoagulates, the retina creating a microscopic spot. Laser surgery, using our Iridex Oculight GL laser, is performed in our office while you are awake and comfortable. The laser is used to seal the leaking vessels within the retina. The laser treatment usually takes less than 15 minutes to complete, and you can go home immediately following surgery. Arrangements for transportation should be made in advance since you may not be able to drive right away. Macular laser photocoagulation was the only available treatment for macular edema in branch retinal vein occlusions from the early 1970s until the early 2000s. Treatment had to be delayed until significant retinal hemorrhages absorbed. Although many patients receiving laser had good visual results, more recent treatments (intaocular injections with anti-VEGF drugs and corticosteroids) have replaced laser as the initial treatment of choice. The macular laser is now mostly used as a way to decrease the number of injections a patient might need.
Macular edema and hemorrhages before laser surgery
Resolution of macular edema 4 months following laser Intraocular Anti-VEGF agents and steroids
VEGF inhibitors (Avastin, Lucentis, and Eylea) and intraocular steroids (triamcinolone, Ozurdex) strengthen the leaky retinal vessels and have become the treatment of choice for macular edema in branch retinal vein occlusion.All 3 VEGF inhibitors are probably equally effective. Unlike laser photocoagulation, vision often improves significantly by 3-4 lines. Patients usually require ongoing injections for maximal results. The laser can be used as a supplemental treatment to help decrease the number of intravitreal injections.
Intravitreal triamcinolone (Kenalog, Triescence) is also effective, especially in eyes that have had cataract surgery, and is associated with a much lower frequency of injections. Sustained release dexamethasone (Ozurdex) can also be used as either a primary or supplemental treatment. Triamcinolone is effective for up to six months and Ozurdex is effective for 2-3 months. Common steroid side-effects include elevated intraocular pressure and cataract.
- Laser Photocoagulation
Retinal neovascularization
Patients should be examined every 4 months to look for the possible development of retinal neovascularization. Panretinal laser photocoagulation (PRP), similar to that performed for proliferative diabetic retinopathy, is performed if neovascularization develops. Laser photocoagulation decreases the chance of developing vitreous hemorrhage (29% with laser vs. 61% without treatment). Additional treatment should be considered if neovascularization persists at the 4-month follow-up examinations.
Some eyes will develop severe vision loss if retinal neovascularization bleeds into the vitreous. Vitrectomy surgery is done in the operating room on an outpatient basis. These advanced microsurgical techniques often allow us to restore vision by removing the hemorrhage and bleeding tissues.
Central retinal vein occlusion.
- Macular edema
Although laser photocoagulation is an effective treatment for branch retinal vein occlusion macular edema, it has no effect on vision in central retinal vein occlusion. Treatment for central retinal vein occlusion macular edema with intravitreal anti-VEGF agents and steroids became available in the 2000s and is very effective, with similar results as with branch retinal vein occlusion. - Iris neovascularization and Neovascular glaucoma
Patients with a new central retinal vein occlusion should be examined frequently during the first 6 months, the period when eyes are at the highest risk for developing iris neovascularization. Close follow-up is particularly important for high-risk eyes (less than one month of symptoms and with those with visual acuity worse than 20/200). Prompt laser panretinal photocoagulation (usually preceded by Lucentis, Avastin or Eylea) should be applied once iris neovascularization develops.Neovascular Glaucoma can sometimes be controlled with anti-VEGF injections and panretinal photocoagulation, although some patients still require glaucoma surgery to prevent severe eye pain or blindness.
- Macular edema
View more retina images at Retina Rocks, the world’s largest online multimedia retina image library and bibliography repository.



