If you have a sandy, gritty irritation or burning in your eyes that generally gets worse as the day goes on, you may have dry eyes, especially if you’ve had these symptoms for 6 months or more. Dry eye syndrome does not truly come and go, but in its early stages, or with mild dry eye, you may only have symptoms after long days, after prolonged computer use, and in dry or windy conditions. In addition, you may notice symptoms only when wearing your contact lenses or when you become dehydrated. The most common treatment for dry eyes is artificial tears, available over-the-counter at your local pharmacy. However, you should always consult with your eye doctor before treating this condition yourself. Other options are available for more severe dry eyes including punctal plugs, medications, and lifestyle changes.
Dry eye is diagnosed with a thorough examination of your eyes with magnifying instruments; measuring your rate of tear production and checking the amount of time it takes for tears to evaporate between blinks. The doctor can also check for pinpoint scratches on the front surface of the eye caused by dryness using special, colored eye drops. At Bennett & Bloom Eye Centers we offer complete, ongoing eye care using the latest technology and techniques to diagnose and treat this condition.
What is dry eye syndrome?
 ‘Dry Eyes’ affects over 10 million Americans and is one of the most common eye complaints of patients. Recent research by the International Dry Eye Workshop defined dry eyes as “A multifactorial disease of the tears and ocular surface that results in symptoms of discomfort, visual disturbance, and tear film instability with potential damage to the ocular surface. It is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface”. In other words, dry eyes can be caused by and worsened by several different factors and it affects both the comfort and the quality of vision as well as the overall health of the ocular surface.
‘Dry Eyes’ affects over 10 million Americans and is one of the most common eye complaints of patients. Recent research by the International Dry Eye Workshop defined dry eyes as “A multifactorial disease of the tears and ocular surface that results in symptoms of discomfort, visual disturbance, and tear film instability with potential damage to the ocular surface. It is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface”. In other words, dry eyes can be caused by and worsened by several different factors and it affects both the comfort and the quality of vision as well as the overall health of the ocular surface.
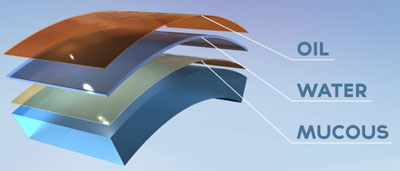
The normal tear film consists of an outer oily layer, a middle watery aqueous layer, and an inner mucous layer. Dry eye symptoms occur when any of these layers are affected. The two most common causes are aqueous deficient and evaporative (due to a breakdown in the outer oily layer that is produced by the lid’s Meibomian glands).
What are the symptoms of dry eye syndrome?
If you have dry eyes, you may experience a sandy-gritty or burning irritation that generally gets worse as the day goes on or after prolonged visual tasks such as computer work, reading, and driving. These symptoms of dryness usually precede watery eyes which then cause blurriness that requires continual blinking to smooth the eye surface and improve vision. These excessive, reflex tears are more watery in nature and are therefore more deficient in some of the other critical components found in healthy tears such as oils, proteins, and mucous. Thus, ironically, a patient can have “watery eyes” but still be diagnosed with “dry eyes” because these reflex tears typically do not coat the eye well, causing residual dry patches on the ocular surface.
How do people develop dry eye syndrome?
Dry eyes develop from either a decreased tear quantity and/or decreased tear quality. Decreased tear quantity (aqueous deficient dry eye) can be caused by increasing age, sex (more common in females), certain medications (including antihistamines, birth control pills, and hormone replacement pills), a history of ocular injury or surgery, and rheumatoid arthritis or lupus (Sjogren’s syndrome). Decreased tear quality (evaporative dry eye) is due to abnormal or decreased lipid secretion from multiple glands in the upper and lower lids (Meibomian glands). This is most commonly caused by decreased gland function with age or a chronic eyelid infection called blepharitis. The quantity and quality of the tear film are also worsened by other environmental factors such as smoking, dusty environments, exposure to forced air (fan or air vents in a car), dry and arid climates (geographical or seasonal with winter heating units), contact lenses, and prolonged visual tasks such as computer work, reading, and driving.
How is dry eye syndrome diagnosed?
Dry eye syndrome is diagnosed by a careful ocular history, slit lamp examination and ancillary testing including corneal staining, phenol red testing, tear breakup time, and Schirmer’s testing.
How is dry eye syndrome treated?
Dry eye treatment is based on the cause(s) of the condition. Based on a thorough history and clinical findings, your doctor at Bennett and Bloom Eye Centers will be able to recommend both lifestyle and environmental changes to achieve the desired results. Our doctors will also incorporate specific eye drops into the treatment plan to help replace the missing tear components to help lubricate the eye, reduce irritation, and decrease reflex tearing. Artificial tears, gel, or ointment work much like hand or skin cream, in that once the dryness is already present it takes several applications for symptoms to completely go away. They also work much better as preventative therapy and should be used on a regular basis to prevent the dryness from returning.
- Artificial tears. Artificial tears and ocular lubricants are available without a prescription. There are many different brands, each with slight differences in their ingredients. Sometimes these drops have ingredients with strong preservatives that may aggravate the problem, so remember that not all tear brands are alike. Consult us before purchasing any of these drops. We prefer the use of tears with either gentle or no preservatives since they are safer to use when applied several times a day. We recommend starting at 6-8 times a day or more, and then backing down to a maintenance dose once you start to notice some relief. Sometimes thicker teardrops or even tear gels may be used to better coat the eye and help natural tears stick to the eye better.
- Serum tears. Artificial tears and commercially available prescription eye drops may not adequately relieve symptoms in some patients. In these advanced cases, autologous serum tears may help. Serum tears are made by a special compounding pharmacy and involve first drawing a patient’s own blood. The liquid part of the blood, the serum, is extracted and eye drops are made from this solution. Serum tears are more similar to a patient’s own natural tears than commercially available drops. They also contain molecules that have anti-inflammatory properties that promote regeneration of the corneal epithelium. Click here to download a handout for further information on using and obtaining serum tears.
- Prescription eyedrops.
- Restasis. For more severe cases other treatments are available. Prescription medications such as Restasis can help reduce the inflammation caused by dryness and even help stimulate natural tear production.
- Xiidra. Approved by the FDA in late 2016, Xiidra is the only medication that treats both the signs AND symptoms of dry eye disease. It reduces ocular surface inflammation in a different manner compared to Restasis. Xiidra is recommended as second-line therapy when over the counter teardrops and lid hygiene practices don’t resolve dry eye symptoms.
- Oral agents. Other oral medications and supplements can help your body make a better quality of tears naturally. Omega-3 fatty acids found in flaxseed and fish oils are one of the more common supplements.
- Punctal plugs and occlusion. We may also recommend closure of the tear drainage system to help keep the tears you do produce in your eyes longer. Just like damming up a river, it stops the current and allows the moisture to pool upon the surface of the eye where it is needed. This can be accomplished with the use of special punctal plugs, which are applied painlessly with a brief in-office procedure. These plugs may be short-acting (dissolve after a few days to see if this treatment works) or more permanent with non-dissolvable plugs. Often a cautery treatment is used instead of the plugs to seal off the tear drain permanently.
- PROKERA. PROKERA is the only FDA-approved therapeutic tissue products that reduce inflammation and promote healing of the ocular surface. It is a biologic corneal bandage device useful for a wide variety of corneal surface diseases including severe dry eye syndrome. Amniotic membranes, which are obtained from the placenta during a planned Cesarean section, have anti-inflammatory properties, promote regeneration of the corneal epithelium, and reduce corneal scarring. Click here for more information about Prokera.
Dry eyes can be an uncomfortable and chronic problem. However, through careful treatment and consistent compliance with your doctor’s orders, symptoms can be significantly relieved if not resolved completely.



