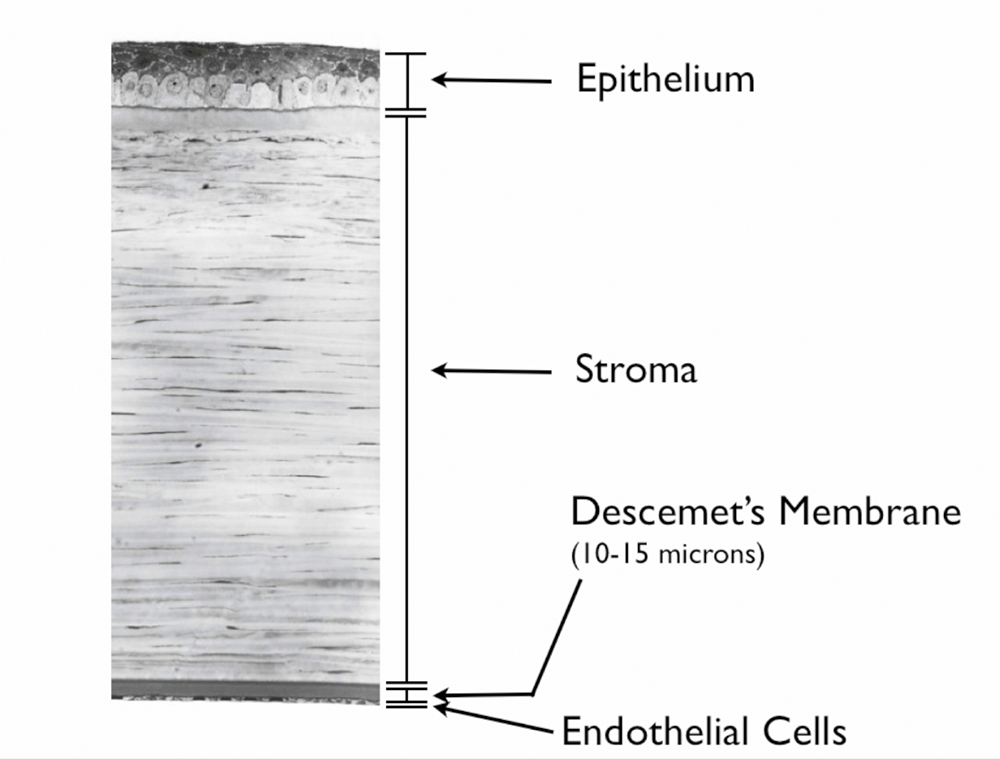
What are the different layers of the cornea?
The cornea is the clear front wall of the eye (similar to a watch crystal). Functionally, the cornea has 3 main layers. Technically, anatomy books may list subset layers to each of these, but for our purposes, there are 3. All layers are clear, and must be so to focus light properly.
The outer 10% or so of the cornea is the protective “skin” layer that has feeling (it tells you to blink when your eyes are dry or if you get something in it). This outer layer is called “epithelium”. The epithelium protects the deeper layers from infection, scarring, drying out, and other potential harm. Just like the outer layer of your skin, the outer layer of your cornea sheds and regenerates itself every week or so, cell by cell. The new cells are grown by “corneal epithelial stem cells”. Therefore, an eye with an area of bad or opaque epithelium that blocks vision, usually does not need a transplant to remove to opacity. Instead the opacity typically only needs to be removed so that new healthy / clear epithelium can grow in from the stem cells. (See superficial keratectomy section). All other layers of the cornea do not regenerate, and would need to be replaced (transplanted) if removed.
The middle layer called “stroma”, for all practical purposes, is “the cornea”, the tough clear front window of the eye that the inner and outer layers serve to protect. It makes up about 85% of the cornea thickness.
The inner layer of the cornea makes up 3-5% of the cornea’s thickness. It consists of up of a thin membrane (like “saran wrap”) that has a single layer of important cells living on it. The membrane is called “Descemet’s Membrane” and the cells are called “endothelial cells”. This layer plays a role in cornea nutrition. The clear fluid that fills the eye is essentially hyper-filtered blood. It flows into the cornea to bring oxygen & nutrients. To prevent swelling or build up of waste products (which would cloud the cornea), Descemet’s membrane prevents the excessive influx of fluid, and endothelial cells continually pump out old fluid & waste products. The inner layer of the cornea prevents swelling (which would opacify the cornea).
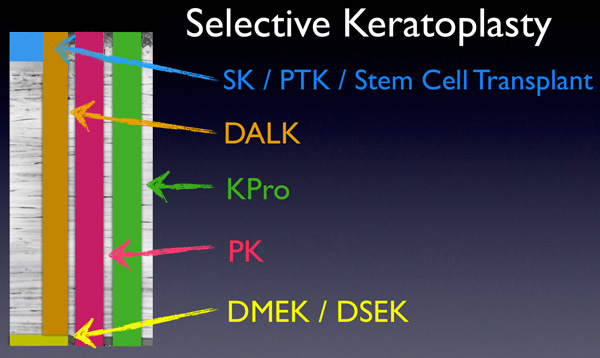
Is it possible to remove and/or transplant just one layer of the cornea?
Yes. We can explain the different types of cornea transplantation using the analogy of a wall. Think of the stroma as the dry wall and bricks, Descemet’s membrane & endothelium as the wall paper, and the epithelium as the temporary protective layers of clear coat that the owner must paint on the bricks from time to time.
Once upon a time, the only type of transplant that was possible was a full thickness cornea transplant or penetrating keratoplasty (PK). With PK, all layers of the cornea are transplanted, and new epithelial cells grow over the new cornea in time. The entire wall is knocked out with a hammer, and a new wall with all it’s layers is brought in. The owner provides a new layer of clear coat over time.
Superficial keratectomy (SK) and photo-therapeutic keratectomy (PTK) remove the epithelium (and possibly some superficial stroma with PTK) so that new healthier epithelium can grow in. The corneal epithelium is the only layer of the cornea that regenerates. SK & PTK are similar to power-washing the outside of the wall. The power-washing typically removes the clear coat and maybe a tiny bit of the outside of the bricks. So, SK & PTK aren’t really transplants. They are like removing some imperfections in the layer of clear coat on the outside of the house so that owner can lay down new clear coat. Conversely, an epithelial stem cell transplant is necessary when the owner’s can of clear coat runs out or goes bad. Here we can give the owner a new supply of clear coat by transplanting in a special area of a donor cornea.
Deep anterior lamellar keratoplasty (DALK) transplants all stroma but leaves the host’s healthy Descemet’s membrane & endothelium behind to allow less risk of rejection or less risk from blunt trauma. This is like removing all parts of the wall, bricks and dry dry wall, etc, but leaving the host’s own delicate wallpaper intact on the inside.
Descemet’s membrane endothelial keratoplasty (DMEK) and Descemet’s stripping automated endothelial keratoplasty (DSAEK) replace Descemet’s membrane & endothelium without removing the host’s stroma. DMEK is more selective than DSAEK. Both DMEK and DSAEK remove old Descemet’s membrane & endothelium. DMEK adds a new Descemet’s membrane & endothelium only. DSAEK adds a new Descemet’s membrane & endothelium with a layer of donor stroma. To use a wall paper analogy: in both DMEK and DSAEK, the old wall paper is removed. With DMEK, only new wall paper is inserted. With DSAEK, a new piece of dry wall that has new wall paper on it is inserted overtop of the old drywall.
Each of these transplant types are discussed in more detail in separate sections.
The image below shows “selective” keratoplasty where only the layer that is sick is treated / transplanted.
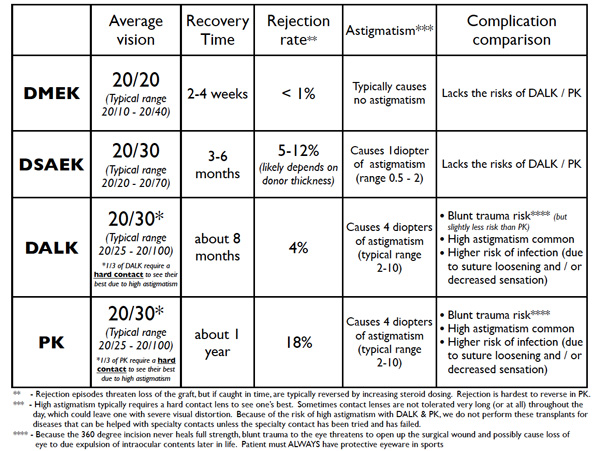
Why do we need different types of transplants? Why not just do PK for everyone and be done?
PK has many limitations regarding vision, astigmatism, recovery time, rejection rate, and other risks. All types of “partial” transplants improve the statistics compared to PK. See table below. DMEK especially has many other benefits compared to DSAEK and PK. (Performing PK for purely endothelial disease is outdated. It would be like knocking down the wall and bringing in a whole new wall when the only thing the wall needed was new wall paper!) More details for each type of transplant are covered in their separate sections.
Do I need do go on systemic immuno-suppressive medications for a cornea transplant?
Not for most types of cornea transplants. Epithelial stem cell transplants are an exception.
When someone gets a kidney or a heart transplant, they need to go on strong medications that make the immune system less aggressive and less likely to attack the transplant. These medications have some potentially significant side effects.
Because there are no blood vessels in the cornea (it is clear!), the cornea is “hidden” from the white blood cells & the immune system to a large extent (with the exception of epithelial stem cell transplants). Thus, for corneal transplants, we only need anti-inflammatory cortico-steroid eye drops to prevent an attack from your immune system (a “rejection episode”). Most patients get down to one drop a day after several few months.
Rarely, patients with aggressive immune systems require stronger systemic medication to prevent rejection. Even with aggressive immune systems, rejection is still very rare with DMEK and is more commonly seen with DSAEK, DALK, or PK. PK has the highest risk of rejection.
After a cornea transplant, do I have to take any precautions if I ever receive a vaccination?
There is some data to suggest that the increase in the immune system activity after a vaccination (such as a flu vaccine, or a shingles vaccine) may put the graft at a slightly increased risk of a rejection episode. To combat this, we typically recommend that if you were down to just one dose of your steroid drop a day, we recommend you increase to four times a day for one week, and then two times a day for one week, and then go back to just one today. If you have previously been told that you cannot take steroid drops due to pressure problems or other issues, do not take it. Instead, ask your cornea surgeon for advice.
How long will my transplant last?
Traditional full thickness corneal transplants last about 15-20 years (give or take depending on the disease type). Endothelial cell count studies show that, with the passage of time, transplants still lose endothelial cells gradually like any other cornea, but usually at a faster rate. When the endothelial cell counts fall low enough, the transplant “fails”. Since DMEK and DSAEK are relatively new, it is not possible to say how long they will last; however, preliminary data is encouraging, especially for DMEK. Many of these transplants will likely last one’s lifetime. But if the endothelial cells of any transplant fails, we can just replace the inner layer (do repeat DMEK for a worn out DMEK, or do DMEK for a PK’s whose endothelial cells have worn out).
Dr. Tenkman is studying variables that may reveal which donors have have cells that are more resistant to death and also surgical techniques are minimally harmful to endothelial cells. Many surgeons suggest it is normal to lose 30-50% of the donor’s endothelial cells during surgery. Dr. Tenkman has some early data suggesting less than 10% cell loss from surgery when selecting a specific subset of donors. We will see how the data pans out over time.
Does a “rejection episode” mean that I will lose my cornea transplant?
No. If untreated, a rejection episode can cause significant damage. But usually the episode stops with an increase in anti-inflammatory eye drops. Patients are instructed to RSVP: come see us if you develop Redness, Sensitivity to light, Vision reduction, or Pain. Such symptoms may be early rejection or other problems. It’s key to see us right away for diagnosis and treatment initiation.
Will I need glasses after my transplant? Could laser vision correction be done to reduce any postoperative need for glasses?
Whether or not you need glasses after your transplant depends on many factors. Some transplants make glasses free vision impossible (sometimes such is the case with PK or DALK, and sometimes even DSAEK). But DMEK transplants are the least likely to block the possibility fo glasses free vision.
Some patients are candidates for ASA (advanced surface ablation) to minimize their dependence on glasses or contacts after cornea transplant surgery. ASA is a laser vision correction procedure similar LASIK. Whether or not ASA could be done to reduce dependence on glasses or contacts after surgery depends on several factors and is taken on a case by case basis.
What are the costs and risks of a cornea transplant?
Corneal transplant tissue is donated, but still typically costs $4,300 or more. The fees go to the eye banks that must harvest the corneas, screen for possible diseases that could be transferred to the patient, transport and process the corneas, and deliver them to the surgery center… all within just a few days. The cost of receiving a transplant includes not just the tissue, but surgery center, surgeon, and anaesthesia fees. Also, organ donors must be tested (and found negative) for every known communicable disease. This testing is costly. Fortunately, the total cost is less at an outpatient surgery center and these costs are typically covered by Medicare and private insurance. Patients can be responsible for deductibles and co-payments. Generally, DMEK and DSAEK can be performed in an outpatient surgery center. DALK and PK more often have to be done at a hospital. Having the surgery at a hospital can increase costs several-fold.
The infection risk of corneal transplantation procedures about as safe as a routine blood transfusion. The risk of receiving a disease from a transplant is very low.
Other risks for transplantaion include: primary graft failure, rejection, graft dislocation, cataract formation, glaucoma, infection, irregular astigmatism, double vision, bleeding, iris damage, vitreous prolapse, cystoid macular edema, swelling, and other complications too numerous to list, including the extremely unlikely possibility of death. Most of these complications are quite rare but are theoretically “possible” with all types of intraocular eye surgery. Patients using steroid drops (which all cornea transplant patients do) have to be followed for the development of high pressure. High eye pressure usually gives no symptoms, so follow up is crucial to allow the doctor to treat any high pressure as necessary with medication or procedures. Patients are usually seen every 3-6 months for life depending on the strength of steroid used.
In our hands, the overall success rate for a DMEK or DSAEK graft attaching well and working is about 99.9%. Should the transplant fail due to rejection or otherwise, it would need to be repeated.
Because the time to heal is longer for DALK & PK, and because they involve more risk, the odds of a DALK or PK failing to restore vision is more significant than DMEK or DSAEK. DALK and PK have several added risks.
- For one, DALK (and more so PK) have a higher risk of bleeding during surgery while the patient’s own cornea is removed and the eye is depressurized. Although not common, such bleeding can do significant damage to the eye.
- DALK (and more so PK) also have a significant risk of rejection. Higher doses of steroid drops may be necessary in here to prevent or treat rejection, which can increase the risk of high pressure (glaucoma) in the eye.
- DALK and PK involve a 360 incision on the cornea. Such large cornea wounds don’t heal with full strength and are at risk to split open with moderate blunt trauma. If the wound were to split open (ie, if a patient fell and hit their face in the shower, or got bumped during a sport), it could lead to loss of the eye. That is why we recommend protective goggles or sun-glasses life-long for any activity that risks bumping the eye.
- DALK and PK require 16 sutures or so. These sutures are not removed for many months or even over a year. The sutures are buried in a manner such that they cause no pain to the patient; however, it is common one of these sutures to become lose. A lose suture can cause a sensation of “sand in the eye”. More so, a lose suture is a risk for infection or “cornea ulcer” (see separate section). Cornea ulcers can be more serious in the setting of a cornea transplant because the immune system in the area is suppressed by steroid eye drops.
- DALK and PK commonly heal with large amounts of astigmatism. Cornea shape determines focus, and astigmatism is a shape anomaly when the cornea is shaped less like a sphere, and more like an egg. Corneal astigmatism is measured in diopters. In routine patients (who have not had had a cornea transplant) we consider 1 diopter “mild” astigmatism, 2 diopters “moderate” astigmatism, and 3 diopters “high” astigmatism. DALK and PK average about 4-5 diopters of astigmatism. A common range is 2-10 diopters of astigmatism. Regarding astigmatism risk, there are controllable and uncontrollable causes of astigmatism. The surgeon can try to sew the graft as evenly as possible to reduce risk of severe astigmatism; however, the surgeon cannot control the natural tension lines in the cornea or how symmetrically the tension lines will balance as the wound heals with a micro-scar. Severe or irregular astigmatism cannot be corrected with glasses, and special hard contact lenses are often necessary. On average, 1/3 of all DALK & PK patients need a hard contact to see their best due astigmatism. Therefore, at Bennett & Bloom, we never perform DALK or PK for keratoconus or irregularly shaped conrea patients to “try to get one out of contact lenses”. The patient could go through all the added cost and risk of surgery only to end up where they started… or worse. DALK and PK are reserved for severe disease that cannot be mended by contact lens wear.
More details for each cornea transplant type are listed in the separate sections.



